[See supplemental article Covid-19, herd immunity and common sense]
TL;DR
- The concept of "Herd immunity" fails elementary rational analysis.
- A "herd" cannot be scientifically defined. A "herd" remains an irreducibly vague concept.
- Ipso facto, "herd immunity" is not an identifiable, valid phenomena.
- Population percentage deaths and illnesses correlate with psycho-social-enviro factors.
When the subject of vaccination1 is discussed within a group (e.g. online forum), and there are some within that group who are pro-vaccination, almost invariably they will at some point raise the issue of herd immunity.
First let's clarify what is meant by "herd immunity"2
From Wikipedia3 this:
"Herd immunity (also called herd effect, community immunity, population immunity, or social immunity) is a form of indirect protection from infectious disease that occurs when a large percentage of a population has become immune to an infection, thereby providing a measure of protection for individuals who are not immune".
There are, it seems to me, a number of aspects to this subject that need clarification:
Firstly, when does a group of individuals become a herd? Is one person, alone, a herd? Clearly not.
What about 2 people, living say within 50 metres of each other? Would they represent a "herd"? Again, few would claim those two individuals would represent a "herd".
The same would be said of say, 3 people living within 440 metres of each other.
We can progress this line of inquiry indefinitely, by including more and more individuals, up to and beyond a community of say, 10, 20 or 50 thousand, or million, or billion and more. As is well-known to philosophers, this line of inquiry is simply another form of the Sorites Paradox4 which, historically, inquired as to how many grains of wheat constituted a heap.5
The Stanford University article (cited above6) draws the conclusion to the paradox, that "This phenomenon at the heart of the paradox is now recognised as the phenomenon of vagueness".
Vagueness?
The Stanford article goes onto to clarify "vagueness" by considering "When does a fertilized egg develop into a person?". In the context of this article, we might also ask "when does a group of individuals become a herd?". Clearly, there are no definable answers to these questions. There is no clear borderline, or threshold for when a collection of grains, or people, become a 'heap' or a 'herd' (resp.). None. Such terms as heaps and herds are, and will remain, irreducibly vague. We may, for example, intuitively assign a particular group of people as a community, but that assignation is an emotional, subjective assessment, not a scientifically, objectively-valid assessment. From afar a group, community, herd or forest might seem a coherent entity, but on close analysis the herd, community or forest all reduce to the identifiable7 individuals within said herd, community, forest. That is, individuality is primary, collectives are secondary, derivative manifestations8.
"Herd immunity" is however considered a very important, real factor for populations remaining disease-free even though what constitutes a "herd" will be invariably vague.
This is the first difficulty with the issue of "herd immunity" — it is by nature an irreducibly-vague subject, yet it is stated as being an essential (non-vague) factor in keeping populations disease-free. One would expect that scientists would be keen to determine the precise nature of when and how the delineation between vague and non-vague occurs, given the pivotal importance in pro-vaccination arguments9.
There is a second difficulty with "herd immunity" — if herd immunity is, as is often vociferously argued, essential to disease prevention, what value is there in individual immunity when an individual strays outside of said "herd"10, when, as a consequence, each vaccinated individual will likely be infected with any disease presented to him/her?
Summarizing the foregoing, we can neither a) clearly define what constitutes a "herd", nor b) when an individual is in a "herd" and thereby supposedly protected by it.
The scientific method involves establishing measurable 1:1 correspondences between cause and effect, and that any such correspondences can be independently replicated. Any linking of some purported cause with that of some effect, that lacks these aspects (1:1 correspondences, replicable, independence) is not regarded as scientific. Given that no one can rigorously claim what constitutes a herd, and what therefore constitutes "herd immunity", asserting that "herd immunity" is essential to disease prevention is clearly a "false conception of causation". This is true irrespective of whatever epidemics, or outbreaks of disease occur, such as for example when a measles epidemic occurs at a theme-park and is believed to be due to a lack of "herd immunity"11.
When people put "trust in magic or chance, or a false conception of causation" they are, in quite literal dictionary-definition terms, putting their trust in superstition12.
Probably. Not!
Now, the foregoing analysis is framed within a black-white, either-or dichotomy — you're either in a herd or not; you're either protected, or you're not. And if you're not in a herd which affords you some protection, then you'll likely be infected with a whole host of diseases.
Of itself that analysis is insufficient for those who believe that one is "more likely" to be protected, the bigger the herd. In other words, the belief is that it's not a black-white situation, but a probabilistic one — that we're more likely (higher probability) of being protected in a herd.
While there's a certain "feel-good" nature to that belief (safety in numbers, etc.) it's not particularly scientific or rational. Nor, I might add, beneficial (it's actually a debilitating belief13).
The belief that one will be "more likely" to be protected via herd immunity involves a neat sleight-of-hand that nearly always goes unchallenged.
To understand that sleight-of-hand, it's helpful to understand the historical background to disease rates.
Dr Suzanne Humphries in her book "Dissolving Illusions" cites hundreds of years of government and medical research that clearly and unequivocally shows rates of infectious diseases were in sharp decline prior to the introduction of vaccines. Let's designate the cause or causes for those declines as being a collective Cause A — in this article it is not pertinent to the analysis to understand the nature of that cause, or those causes, but that something caused the decline.
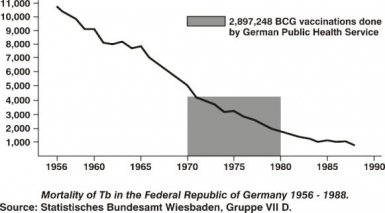 Let's (for the moment) assume vaccination was effective, and designate its role as Cause B (for the decline in the rates of infectious disease).
Let's (for the moment) assume vaccination was effective, and designate its role as Cause B (for the decline in the rates of infectious disease).
As Humphries reveals, disease rates had fallen by around 80 - 98% prior to vaccines, due to what I have designated as a collective Cause A. Cause B (vaccines) was (at best) a co-factor within the trajectory of decreasing disease rates (see figure right, which is typical of the decline in disease rates within developed, Western economies).
Based on probabilities it would be far more prudent and beneficial to rely on the clear majority factor, Cause A, than rely on a minority factor Cause B (with documented side-effect risks).
The "sleight of hand" mentioned earlier is that the idea of being "more likely" to be protected in a herd, relies on the assumption that vaccination is responsible for the decline in disease rates. As the figure (above right) shows, that's an assumption that fails scientific scrutiny — the graph shows Cause A at work, and Cause B as incidental, without noticeable effect14. As per the above definition of superstition, believing that vaccines and herd immunity offer protection, sans scientific evidence, is a superstition while ever Cause B remains under the purview of Cause A15.
I would have thought any concerned, responsible parent or medical professional would avoid "like the plague" unfounded, speculative beliefs where matters of health and wellbeing of children are concerned.
Update, additional
In discussing the probability-issue with a highly-intelligent friend, he explained there's two additional aspects to probabilities that I had not covered: severity and variability.
 As to the first - severity relates to the severity of outcomes. For example, a mild cold is far less severe than pneumonia. In this article, I cite references that typically involve mortality (100% severity), for ease of clarification.
As to the first - severity relates to the severity of outcomes. For example, a mild cold is far less severe than pneumonia. In this article, I cite references that typically involve mortality (100% severity), for ease of clarification.
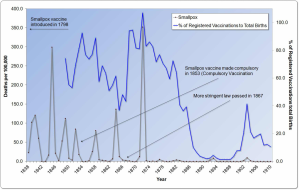
As to the latter, my friend argued that if variability of rates of disease went down/was lower after vaccinations, that would indicate a high level of efficacy, of said vaccines. In her book "Dissolving Illusions", Dr Suzanne Humphries cites around 500 medical journals and government reports. In the graphical analyses she presents, variability of disease rates INCREASE (see figure right) after the introduction of vaccines, even while the mortality-rate is decreasing, in line with the decrease that was already occurring prior to vaccines.
Of particular note is (as per diagram above right16) how disease rates were lower when the percentage of those vaccinated decreased and the lower variability (or swings in rates) with the decrease in percentage vaccinated. Note the small "blip" of increased rates of disease with the increased rates of vaccination at ~1894, and again at ~ 1903-1904.
Note also that after the "more stringent law" for vaccination was passed in 1867, mortality (deaths) increased markedly, in line with the increased percentage of those vaccinated. Compare with the period 1890 - 1902, when very few were vaccinated, and there was near-zero deaths from smallpox.
H=1-(1/R0)
Another approach is to consider how scientists and medical personnel calculate herd immunity "H" (via the formula H=1-(1/R0)).
R0 is the rate of spread of contagion from one individual to others. For example, for highly infectious diseases like measles, R0 is 15. Meaning that H = 1 - 1/15 = 93.4% of the population need to be immune, in order to achieve "herd immunity".
However, as is more fully detailed in this article, research spanning 30+ years by Sir Prof. Michael Marmot and others have found that:
"Where you stand in the social hierarchy is intimately related to your chances of getting ill, and your length of life ... The higher the status in the pecking order, the healthier they (you) are likely to be. In other words, health follows a social gradient. I call this the status syndrome."17
Prof. Len Syme adds,
“psycho-social factors are related to the vulnerability and defences that people have to disease, not to what disease you get. So that these factors affect the body's defence systems and make you vulnerable to smoking and cholesterol and viruses18 and so on.”19
In other words, highly positive psycho-social factors—a high degree of ease, status, financial and emotional stability, confidence, belief, social engagement, etc20—will, in effect, provide a bulwark for those who are healthy, wealthy and emotionally wise. That is, their high-status, health and wealth will offer them a "natural immunity" to disease.
Arguably, if sufficient attention was directed to improving psycho-social factors, an R0 of 1, which would deliver a herd immunity of 0% of the populace needing vaccines, could be readily achieved, relegating vaccines as unnecessary, and given the documented side-effects, ill-advised. In that scenario, "herd immunity" (the subject of this article) would be rendered irrelevant. In short, a populace with high level of autonomy, equality, ease, fulfillment, social engagement, purpose, etc, would give herd immunity to dis-ease (disease) without the need for vaccines.
Update February 8, 2017 - Another approach
I came across this post "Herd Immunity: Junk Science at its Finest", which provides an additional approach highlighting the fallacy of herd immunity.
In particular (Dr. Russell Blaylock MD, a retired neurosurgeon):
When I was in medical school, we were taught that all of the childhood vaccines lasted a lifetime. This thinking existed for over 70 years. It was not until relatively recently that it was discovered that most of these vaccines lost their effectiveness 2 to 10 years after being given. What this means is that at least half the population, that is the baby boomers, have had no vaccine-induced immunity against any of these diseases for which they had been vaccinated very early in life. In essence, at least 50% or more of the population was unprotected for decades.
If we listen to present-day wisdom, we are all at risk of resurgent massive epidemics should the vaccination rate fall below 95%. Yet, we have all lived for at least 30 to 40 years with 50% or less of the population having vaccine protection. That is, herd immunity has not existed in this country for many decades and no resurgent epidemics have occurred.
Vaccine-induced herd immunity is a lie used to frighten doctors, public-health officials, other medical personnel, and the public into accepting vaccinations.”
Regression into wishy-washy conjecture
In light of the foregoing –that we cannot define a herd– the following conversation is one example of the response to that dilemma:
Me: "So, Andy, what would you define as a herd of people, how many specifically?"
Andy: "I'd say 150 people."
Me: "Okay, that would mean 149 people in a community would not constitute a herd, correct?"
Andy: "No, it's the qualitative aspect, which means that herd immunity is still important."
Notice the segue – from a very definable and measurable quantity to the immeasurable aspect of quality.
Since quality cannot be directly measured the conversation had slipped into wishy-washy conjecture – a highly-emotive subjectivity sans scientific rigour. All of which again confirms the baseless nature of "herd immunity" as a determinant of disease prevention.
As John Lasschuit clarifies (correctly, in my opinion):
You measure quantity, not quality. As soon as you measure, you're quantizing. You are defining fixed segments of an unlimited source, and by defining those segments, you automatically leave out an unlimited number of aspects which together form what we experience as quality. You can measure quantity, but it's impossible to measure something undefined as quality.
- 1. For the purposes of this article "vaccination" is used in the ideal case whereby each vaccination creates immunity. This equivalence is deliberate in order to avoid distractive arguments that are not relevant to the analysis of "herd immunity" using the Sorites Paradox.
- 2. For the purposes of this article "vaccination" is used in the ideal case whereby each vaccination creates immunity. This equivalence is deliberate in order to avoid distractiions that are not relevant to the analysis of "herd immunity" using the Sorites Paradox.
- 3. While Wikipedia is often not considered a credible resource, this article provides an analysis relating to perceptions typically voiced.
- 4. Sorites Paradox, Stanford Encyclopedia of Philosophy.
- 5. As is covered in the Stanford University page, and other similar articles on the Sorites Paradox, if one proposes that (in respect of this article) a herd is, for example, 1000 people, then a community of 999 will not be a "herd" and can not therefore provide any immunity, whatsoever. If, in response, one where to argue, "oh, well, 999 is also a herd, and can provide herd immunity", then by that logic, so can a community of 998, and 997, and 996 ... and, continuing the sequence, and in direct contrast to the first consideration raised in this article, we end up with a "community" of three, then of two and finally, a "community" of one. But how does 80-95% of an individual provide "herd immunity" to themselves? Perhaps, as Prof. Sir Michael Marmot, Prof. Len Syme and others have found, if one is 100% fit within oneself (psycho-socially) then yes, indeed, one can confidently expect they will be immune to disease, no matter what its nature or origin.
“psycho-social factors are related to the vulnerability and defences that people have to disease, not to what disease you get. So that these factors affect the body's defence systems and make you vulnerable to smoking and cholesterol and viruses and so on.” [Prof. Len Syme, University of California].
- 6. Sorites Paradox, Stanford Encyclopedia of Philosophy.
- 7. countable, measurable
- 8. Fundamentally, all collectives are secondary manifestations reliant on individual choice and cooperation, irrespective of however that cooperation is achieved, e.g. by force or via other means
- 9. And, as one reader (Leah) pointed out, even within communities where all the children are vaccinated, adults also (obviously) comprise that community, and yet how many of those adults are fully vaccinated, with regular booster shots and the like? The unknown percentage of adults who remain unvaccinated, or lapsed-vaccinated in such communities would clearly undermine the validity of "herd immunity" even if one were able to somehow clearly define what constitutes a "herd".
- 10. when said herd, see the first point, cannot be clearly and unambiguously defined, in any case.
- 11. Same applies for any other outbreak of disease.
- 12. "superstition" derives from the Latin "superstitionemin" which means a "(religious) belief based on fear or ignorance and considered incompatible with truth or reason". Accordingly we may consider "herd immunity" a bone fide superstition.
- 13. For a similar reason of feeling that remaining on the sinking Titanic would be safe if all passengers were to bunch together, in a "herd".
- 14. Note how the graph shows the rate of decline in mortality is, in the midst of the introduction of vaccines, worse than the previous high-rate of decline in deaths.
- 15. Validation of Cause B as instrumental in disease prevention necessitates Cause A being entirely removed from, or fully calibrated within the scope of Cause B. No such research (to my knowledge) has been conducted, nor I expect is likely to be conducted while ever vaccines remain a profitable avenue for the medical and pharmaceutical industries.
- 16. A full list of all graphs used in "Dissolving Illusions" is available online.
- 17. Michael Marmot, The Status Syndrome: How Social Standing Affects Our Health and Longevity, Holt Paperbacks, 2005, p.1
- 18. my emphasis
- 19. Prof. Len Syme, with Norman Swan “The Health Report: Mastering the Control Factor: Part One [transcript]”, ABC’s Radio National's The Health Report (9 November, 1998) introducing research conducted by Dr Michael Marmot.
- 20. The 9 key factors in overcoming terminal illness would best be adhered to, or adopted in cases of any illness